Fibromyalgia Basics
Acupuncture From East to West

What comes to mind when you hear the word “acupuncture?” Your answer is probably needles, and you may think: I’m already in so much pain … why would I want to have needles stuck in me? It turns out, acupuncture can be quite relaxing and pain-reducing for many people.
Acupuncture is now widely used in the United States to treat an array of painful conditions, including fibromyalgia. David Bilstrom, M.D., a physical medicine and rehabilitation specialist in Chicago, IL, says that “acupuncture can play a very important role in the treatment of fibromyalgia.” If you want to give it a try, this article explains the science, what to expect from a session, and how to find a provider.
The Basics
Acupuncture, which originated in China about 2500 years ago, is one of the most common forms of medicine worldwide. Although the techniques have changed over time with the influence of different cultures and generations, the same basic principles apply.
Dispersed all over the body, there are hundreds of precise locations, or “points,” believed to be sensitive to acupuncture. During treatment, a practitioner chooses some of these points (usually anywhere from 12-35) in which to insert ultra-thin, sterile, stainless-steel needles. Before you are dissuaded, remember, these are NOT like the hypodermic needles that are used to draw blood or administer trigger point injections!
“Acupuncture needles are actually about as thin as two hairs put together and are dull tipped,” says Bilstrom. “When placed into the body, they simply part the skin and the tissues. A person may not even feel the needles as they go in, and if they do, it’s usually a relatively minor, transient sensation. This can be an itch, ache, warmth, tingle, or electrical sensation that radiates a short distance up or down from the point.” Sometimes, to further stimulate acupuncture points, a mild electrical current is applied to needles. This type of treatment is called electroacupuncture.
In the United States and other Western nations, more patients are integrating acupuncture into their healthcare regimens, most of whom are seeking relief from pain. In 1997, the National Institutes of Health reviewed the evidence on acupuncture and pronounced that it may be beneficial for the treatment of several disorders. For fibromyalgia, they determined that it could be useful as a complementary therapy (as opposed to a stand-alone therapy).1 The acceptance of this Eastern practice continues to grow, but just how do these tiny needles improve health?
Eastern Point of View
Traditional Chinese Medicine (TCM) is based on principles taught in most Eastern medical schools. At the core of TCM is the premise that there is a “life energy,“ called “Qi” (pronounced “Chee”), that runs through each person in channels called “meridians.” Just as blood flows through the circulatory system, Qi flows through meridians. When this energy flow is disrupted, health problems occur. Pain, which is viewed as a symptom in Western medicine, is considered a disease itself in TCM.2 So, fibromyalgia is viewed as an obstruction of Qi and blood flow.3
To correct the flow of Qi, specifically mapped points along meridians are stimulated. Based on their diagnosis, practitioners stimulate particular points with heat, pressure, suction, or needles (most common). Acupuncture needling works to release the blocked Qi by tapping into meridians. When energy flow is normal, symptoms dissipate. Although this explanation for disease may seem quite abstract, research studies provide a clearer picture of the mechanisms at work.
What does the Research Reveal?
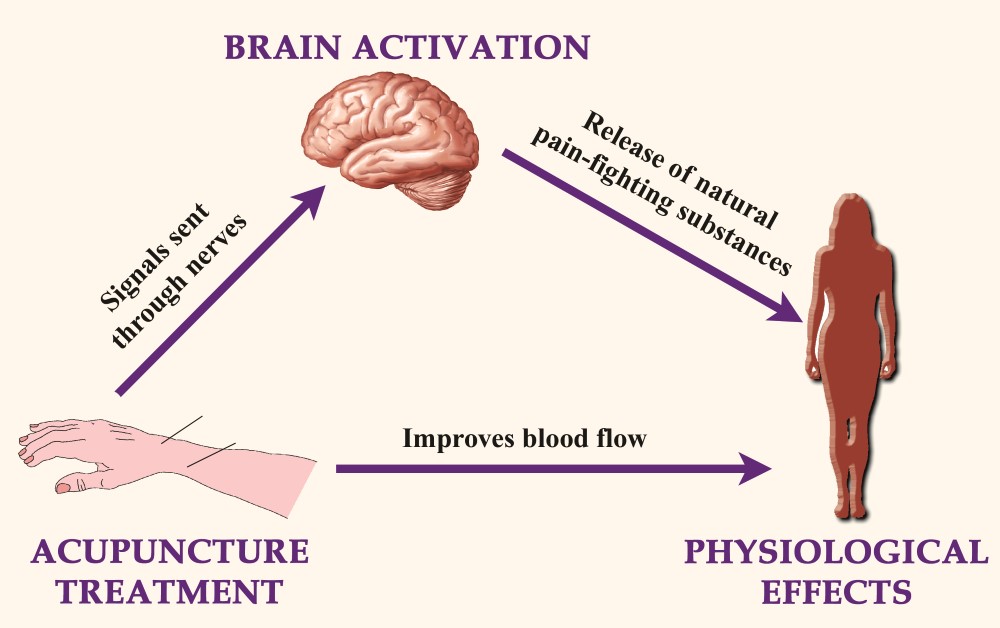
If you visualize the nervous system, it is easier to understand how acupuncture exerts its benefits. The brain communicates with the rest of your body through an intricate nerve network that stretches all over. Acupuncture needles stimulate these nerves, which send signals to your brain. Of course, the brain influences the body’s overall health. As illustrated below, needles stimulate nerves in the body, sending signals to the brain, which in turn cause the release of pain-fighting substances. In addition, acupuncture increases blood flow.
One report indicated that substances that are known to reduce pain, such as the body’s natural opioids (e.g., beta-endorphin and enkephalin) and serotonin, are increased after acupuncture treatment.4 Supporting the role for natural opioids in acupuncture’s analgesic effects, another study showed that blocking the opioid receptors prevented the pain relief that this therapy provides.5
Acupuncture & Fibro
Studies show that acupuncture treatment can address various fibromyalgia anomalies. Haiko Sprott, M.D., of Switzerland, found that microcirculation is impaired in fibromyalgia patients, and blood flow to the tissues is reduced.6 This reduced circulation may be a source of pain. In another study, Sprott demonstrated that acupuncture increased blood flow over tender muscle areas, reducing their number and the degree of pain that they produced..7
Serotonin, a natural pain reliever, is unusually low in people with fibromyalgia. Sprott measured this transmitter before and after acupuncture. He found that increases in serotonin represented an objective parameter for demonstrating the efficacy of this treatment in FMS.8 This may be another way that acupuncture relieves pain.8 Overall, the pain in the fibromyalgia patients was decreased by 45 percent.
How do needle placement and stimulation influence the success of acupuncture for fibromyalgia? One study addressed this question by varying points and the use of manual manipulation in a group of patients.9 Pain was significantly reduced in 25 to 35 percent of patients and did not seem to depend on needle location. The researchers speculated that there may not be “incorrect” acupuncture points for fibromyalgia patients because pain is widespread.
This idea is supported by another study using electroacupuncture for fibromyalgia.10 Treatment was individualized to the patient (points were chosen based on specific symptoms). Many patients reaped significant improvements in sleep quality and pain levels. The results of the study also suggest that adequate depth of needle insertion and electrostimulation may be two important factors in treatment success.
Keep in mind that acupuncture treatment can address a variety of healthcare concerns. “Many people that come to see me primarily ask for assistance with fibromyalgia pain,” says Bilstrom. “What many of them don’t know is that it can be quite helpful with other difficulties that patients experience, such as IBS, headaches, acid reflux, fatigue, and insomnia. One of the things that is wonderful about acupuncture is that it can help control the underlying ‘imbalance,’ and helps multiple symptoms all at the same time.”
Finding a Provider
There are roughly 15,000 acupuncturists in the United States, one-third of which are medical doctors (M.D.s or D.O.s). When looking for a provider, you have the choice between a physician or a licensed acupuncture practitioner. It all depends on what you are looking for. One key attribute to seek out in any provider is experience: “You want to look for a physician acupuncturist who sees quite a few patients,” says Bilstrom. “With non-medical doctors who provide acupuncture, you want to look for either a licensed acupuncturist (L.Ac.) or an oriental medical doctor (O.M.D.). To be certified as either, a significant amount of training is required.”
Physicians and licensed acupuncturists differ in a few ways. Physicians largely employ Western training while licensed acupuncturists employ Eastern training (TCM). Most physicians used medications for pain along with acupuncture treatment, while licensed practitioners were more likely to use other tools of TCM, such as heat, herbs, or moxabustion (the burning of a Chinese herb on acupuncture points). Roughly 85 percent of each group recommended massage, but the licensed acupuncturists were more likely to administer this therapy themselves.
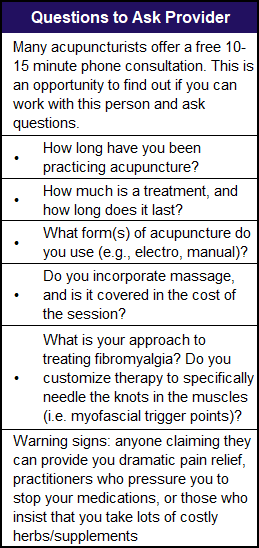
Before locating a provider, you should contact your insurance company to find out what they cover and what restrictions they may place on providers (see last section). In addition, there are websites at the end of this article. Once you have a potential provider on the phone, see the last section on: Questions to Ask a Provider.
What to Expect

After selecting a practioner, what should you expect on the day of the treatment? “The typical acupuncture session entails a thorough review of the patient’s history as well as a complete physical examination,” says Bilstrom. “I usually spend an hour and a half with each patient on the first visit.” After the initial assessment, Bilstrom says, “The actual acupuncture treatment typically lasts between 10 and 20 minutes.” After the session, he adds: “It is nice to just let the body relax and respond as well as possible to the acupuncture treatment, so patients should take it easy for the rest of the day.”
You might wonder how many sessions you will need to notice improvement. For new patients, Bilstrom says, “I recommend to people that they initially be seen once a week for at least six weeks. If there is no significant change in the first six visits, I then recommend stopping the treatments, as they are likely not responders to this therapy.” For those who do respond within six sessions, Bilstrom recommends weekly visits until maximum improvement is reached followed by “booster treatments.”
Cost and Insurance Issues
Acupuncture has potential but the main drawback is cost. Much like other areas of healthcare, this therapy is not cheap. The first visit includes evaluation as well as a treatment, although following visits are less costly. For a licensed practioner, expect to pay between $100 to $200 for the first visit and $50 to $75 for subsequent visits. If you go to a medical doctor, these costs can double, but you are paying for the office visit as well.
An increasing number of insurance companies are covering acupuncture treatments, so you may not have to pay out-of-pocket. Each health plan is different, and insurance company guidelines differ from state to state. Be sure to contact your insurance provider to ask about coverage. Below are some important questions to bring up:
- Do acupuncture visits need to be preauthorized?
- Do I need a referral from my primary care doctor?
- How many visits are covered?
- Is there a copayment? If so, what is it?
- Will acupuncture be covered for any condition? (If not covered for fibromyalgia, ask about other conditions you have, such as headaches, IBS, low back pain, etc.)
- Do I need to see an acupuncturist in your network?
- Will visits to any licensed practitioner be covered (in other words, does the provider have to be an M.D. or D.O.)?
For answers to many financial questions about acupuncture, visit the NIH’s National Center for Complementary and Alternative Medicine at: http://nccam.nih.gov/health/financial.
If you are interested in trying acupuncture, call your insurance provider before selecting a practitioner. This may help minimize your out-of-pocket costs. In choosing an acupuncturist, bring up the questions listed below. Keep in mind that it may take up to six treatments before you notice improvements, after which you will be able to decide whether acupuncture is a worthwhile addition to your healthcare.
Resources for Finding an Acupuncturist
Medical acupuncturists (M.D.’s or D.O.’s)
● may combine other forms of Western medicine
● insurance more likely to cover visits
● more expensive if paying out of pocket
Search for a provider at the American Academy of Medical Acupuncture’s website at
www.medicalacupuncture.org.
Licensed practitioners (L.Ac.’s, O.M.D.’s, or D.O.M.’s)
● based in TCM; may combine herbs and massage into treatment
● best bet if paying out of pocket
Search for a provider at the National Certification Commission for Acupuncture and Oriental Medicine’s website at
www.nccaom.org
1. NIH Consensus Panel. JAMA 280(17):1518-24, 1998.
2. Eshkevari L, Heath J. Holist Nurs Pract 19(5):217-21, 2005.
3. Zheng L, Faber K. Curr Pain Headache Rep 9(5):307-12, 2005.
4. Cabyoglu MT, et al. Int J Neurosci 116(2):115-25, 2006.
5. Mayer DJ, et al. Brain Res 121(2):368-72, 1977.
6. Morf S, et al. Arthritis Res Ther 7(2):R209-16, 2005.
7. Sprott H, et al. Wien Klin Wochenschr 112(13):580-6, 2000.
8. Sprott H, et al. Rheumatol Int 18(1):35-6, 1998.
9. Harris RE, et al. J Altern Complement Med 11(4):663-71, 2005.
10. Deluze C, et al. BMJ 305(6864):1249-52, 1992.
