Possible Causes
Chemical Imbalances
The chemical alterations in the CNS are the target of many treatments prescribed for fibromyalgia, so it’s important to understand their role in this disease.
The spinal fluid provides a window into the cord’s activities and it can also influence what happens in the brain because this liquid bathes all the centers “upstairs.” Most pain-amplifying substances are three-to-four times that of healthy people, while the pain-inhibitors are greatly reduced except for opioids.
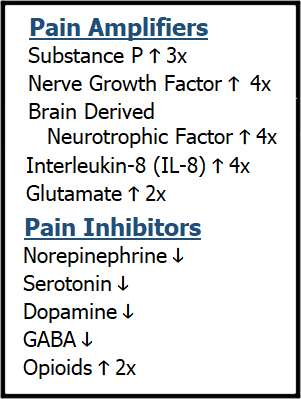
Despite your widespread pain, your spinal fluid level of opioids is double that of normal. Some might say that fibromyalgia patients won’t benefit from taking an opioid because their bodies are already producing plenty of this analgesic. In reality, your system is working overtime to shut down your pain by pouring out opioids. However, your opioids are no match for the dramatically increased concentrations of pain-amplifiers, especially given the low level of other pain-inhibitors.
The Bottom-Up system uses GABA, a nerve calming transmitter to reduce the strength of signals traveling up the cord, along with opioids. Alternatively, this system can amplify signals to get the brain’s attention by releasing glutamate. As you will note from table above, the spinal fluid in fibromyalgia patients contains a twofold increase in glutamate, while GABA is low.
The Top-Down system is best known for its ability to pump out the body’s naturally produced opioids when a person is seriously injured. In addition to opioids, it uses a network of neurons that release serotonin, norepinephrine, and dopamine to provide analgesia. The Top-Down controls can intercept signals entering the cord and, if that doesn’t work, it can modulate the transmissions at the level of the brainstem as well as the lower brain regions.
Given that serotonin, norepinephrine, and dopamine are low in the spinal fluid of fibromyalgia patients, the Top-Down controls are thought to be inadequate. But why are these pain-relieving transmitters low when you are in so much pain? For reasons unclear, your CNS is not making enough of these substances. Maybe your brain is misinterpreting the situation or perhaps it is due to your genetics. This is a complicated situation that researchers have yet to figure out.
Naturally, you are probably wondering about the abundance of pain-enhancing chemicals. Why so many and where do they come from? The transmissions coming in from the peripheral tissues can release substance P and other pain transmitters into the spinal cord. But before the signal enters the cord, it goes through the bulb-shaped ganglia that can greatly increase the release of these chemicals into the cord. And don’t forget the glia (the immune cells that are partners in crime with your neurons). They can control the production and release of these pain-enhancers.
Rather than lumping the Bottom-Up and Top-Down systems together, it is important to understand that each one may use different neurotransmitters and this impacts treatment. Medications that boost CNS levels of GABA (such as gabapentin and pregabalin) work primarily to improve the functioning of the Bottom-Up system, while medications that increase serotonin and norepinephrine (such as duloxetine, Savella or amitriptyline) bolster the Top-Down system. However, there is an overlap in the use of transmitters by these systems.
Strategically, it makes sense to treat fibromyalgia by simultaneously improving the function of both pain control mechanisms. Conversely, taking a second medication that works on the same system is not likely to be beneficial. More details about your treatment options are provided in the Fibromyalgia Basics section of this website.
The table above clearly depicts an imbalance in CNS chemicals in people with fibromyalgia, but keep in mind the following caveats regarding some of the messengers:
GABA – Highly Sedating – While drugs that increase GABA in the cord can reduce your pain, too much of this transmitter will make you groggy.
Serotonin – Can be Good & Bad – This transmitter is often viewed as a “feel good” chemical. However, when serotonin is released into the synapse, it can activate a receptor that leads to increased transmission of pain or one that leads to a reduction in pain. Taking a drug designed to boost the amount of serotonin at all synapses is akin to playing Russian Roulette (i.e., most drugs on the market).
Norepinephrine – A Delicate Balance– Increasing this transmitter can reduce pain and fatigue. Unfortunately, the activating nature of this transmitter can also destroy sleep.
Dopamine – Insufficient & Overlooked– Not only does dopamine relieve pain, but it also improves cognition. Low levels in the CNS likely contribute to brain fog in fibromyalgia (i.e., fibrofog), but dopamine enhancing drugs are seldom prescribed.
Opioids – High Levels Spell TROUBLE – The downside of chronically elevated opioids in the spinal fluid is the activation of immune system glia, which leads to the secretion of nerve-irritating chemicals (increasing pain). This mechanism can be beneficial in the short term for snagging the brain’s attention to get the pain under control, but on a chronic basis it may spell trouble.
Substance P, Nerve Growth Factor (NGF), Brain Derived Neurotrophic Factor (BDNF), and Interleukin-8 (IL-8) – These heavy-hitters are close to a fourfold increase in your spinal fluid, giving them the power of a sledgehammer to knock you around and make you miserable. Most of them are released into the cord by incoming sensory signals. Not only do they ramp up your pain, they also contribute to sleep disruption and fibrofog. Unfortunately, there are no medications or therapies that can cut them down to size … at least not yet.
