Fibromyalgia Basics
What’s Driving Your Pain?

The 18 tender points that were used to diagnose fibromyalgia are more than just sore areas on the body of patients. Ninety percent are actually myofascial trigger points (MTPs), according to an AFSA-funded study by Hong-You Ge, M.D., Ph.D., of Aalborg University in Denmark.1
Importance of MTPs
Why is Ge’s finding so important and what does it matter if the painful areas on your body are called tender points or myofascial trigger points? Tender points were just viewed as “sensitive” areas. They were never thought to be associated with any objective abnormalities. Pressing on tender points simply confirmed that you hurt in multiple areas; they did not explain why you have diffuse pain all over. On the other hand, MTPs can be imaged and are known to contain pain-sensitizing chemicals.
You can probably locate some of your MTPs by manually touching or feeling for them. They are the hard nodules in tight, ropy muscle bands that shorten the muscle and restrict movement. The ability to locate MTPs by pressing on the muscles (palpation) can vary depending upon the experience of the examiner. Fortunately, with the use of intramuscular electromyography (EMG), Ge was able to objectively identify the MTPs in 30 fibromyalgia patients used in his study.
EMG involves inserting a small, thin needle into the MTP (located first by palpation) and measuring the electrical activity in the region. Even though surface electrodes prove the muscles examined are at rest, the needle EMG measures the amount of electrical activity in the area. MTPs generate a substantial amount of electrical activity, and the needle of the EMG can pick up these electrical signals to confirm their location.
MTPs consume energy to maintain their tightly contracted and knotted state. In the process, they also give off a continuous stream of electrical signals. However, once the needle is inserted far enough into the heart of the MTP, it releases the contraction and the electrical signal on the EMG drops to nothing. In fact, this is the same mechanism used by a technique called dry needling to relieve MTPs (in other words, to treat the MTP so that the muscle can fully relax).
Understanding MTPs
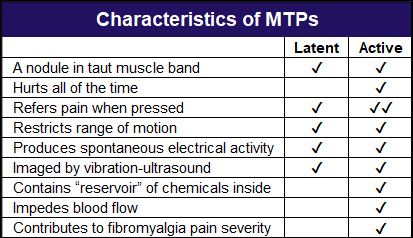
There are two types of MTPs: active and inactive (latent). Active MTPs hurt without pressing on them or moving the muscles that they reside in, and they should be the focus for treatment (see table below). Although latent MTPs can restrict range and hurt when pressed as well as radiate or “refer” some pain to other muscles, they do not spontaneously generate pain. Keep in mind, however, that overusing muscles can easily convert latent MTPs to actives.
While the goal of Ge’s study, funded by AFSA, was to evaluate the 18 tender point locations to assess whether they were MTPs, he also looked at factors that contributed to the severity of fibromyalgia pain.
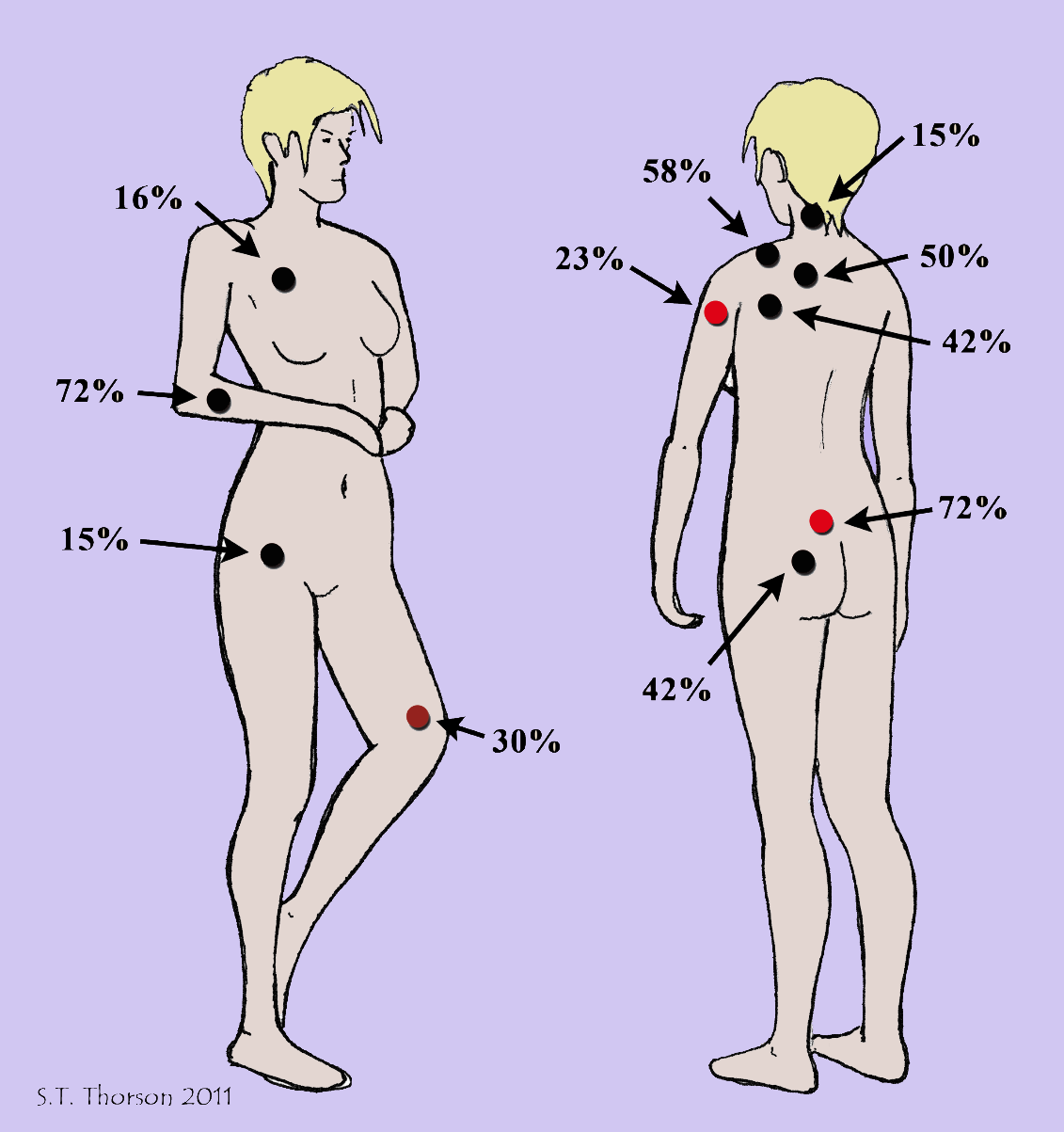
The discomfort generated by the MTPs at the predefined tender point sites produced most, but not all of the pain felt by the fibromyalgia patients in the study. So, other areas with active MTPs are likely adding to your discomfort, such as those in the mid to low back and the upper arms. After all, the 18 tender point sites were selected to standardize research and probably will not include all the trigger points that are contributing to your pain.
The diagram below shows the areas where Ge found the most common MTPs in fibromyalgia patients. The black dot areas coincide with 18 tender points (or they are nearby), while the two red dots were also commonly found in patients. In fact, the low back MTP was the most prevalent, and it was not included in the initial diagnostic exam of fibromyalgia patients.
Looking at the relationship between MTPs and each patient’s pain severity index, Ge found that the total number of active MTPs predicted the person’s pain level. In other words, as the number of active MTPs increased, so did the person’s pain severity. The number of latent MTPs had no effect on each patient’s overall pain rating.
Although the muscle fibers at a latent MTP have just begun to constrict and form a nodule, an active MTP appears to be much more evolved. A buildup of nasty chemicals (like a “reservoir”) exists at active MTPs. These substances can irritate nerve endings and likely explain why they produce spontaneous pain, even when you are not moving.2 Blood flow through the active (but not latent) MTPs is also impeded.
MTPs are not just areas in the muscle where the fibers are contracted and the chemicals are shored up, they also generate electrical activity. This is key. The electrical signals produced by MTPs are transmitted to the central nervous system and can keep it “fired up.” So not only do active MTPs hurt, but they also rev up the central nervous system, which then sends amplified signal to other muscle groups.
Ge’s study shows that the muscle tissues are important contributors to the pain of fibromyalgia. Active MTPs may possibly be a source of electrical input that maintains your dysfunctional central nervous system state. And once this happens, the nervous system sends out signals to the muscles, which may lead to the development of more MTPs.
Patient Recommendations
“Active MTPs are important pain generators in fibromyalgia,” says Ge. “Targeting active trigger points should significantly relieve fibromyalgia pain and represents a promising treatment potential.”
Although 90 percent of the predetermined 18 tender point sites were found to contain MTPs, not all of them were of the “active” variety. Muscles in the back shoulders, buttocks, and upper forearm regions were most likely to contain active MTPs, but this is only based on the 18 tender point sites. “Examining physicians should check active MTPs in all muscles according to a patient’s pain drawing,” says Ge.
There are many ways that practitioners can help you find and relieve your active MTPs. However, unless you also address the perpetuating factors that caused the development of the MTPs in the first place, they will probably come back. For example, repetitive motions, nutritional deficiencies, cold and drafty environments, an underactive thyroid, disturbed sleep, chronic or recurring infections, and prolonged tension may hamper your treatment progress.
The good news is that MTPs are structural anomalies in the muscles of fibromyalgia patients that can be corrected to varying degrees by a variety of techniques. “Relief of active MTPs would decrease fibromyalgia pain intensity and significantly reduce the input that maintains the dysfunctional nervous system,” says Ge.
“Before long-term pain relief is obtained, perpetuating factors for the development and maintenance of MTPs must be resolved,” says Ge. “In this respect, acute and chronic muscle overload can easily cause pain reoccurrence. MTP therapy should be continued at some regular interval (once a week, once a month, etc.) tailored to each patient. If pain in one body region returns, this is a good indicator for seeking immediate treatment.”
In addition to getting professional help with deactivating your MTPs, you should have a daily home program that helps reduce muscle tightness and pain. Submerging your body in soothing warm water (or applying a moist hot wrap to troublesome areas) can relax muscles and open blood vessels to enhance circulation. Even if you cannot afford regular visits to the massage therapist, an electric massager with a long handle and swivel head may offer relief. The goal is to keep your muscles as healthy and functional as possible.
Trapezius Good Starting Place
If active MTPs in multiple muscles are the likely driving force for your widespread fibromyalgia pain, where should initial treatment be focused? One possibility might be your trapezius, the large shoulder muscle located in your upper back region. It’s a troublesome area that most all fibromyalgia patients state is painful.
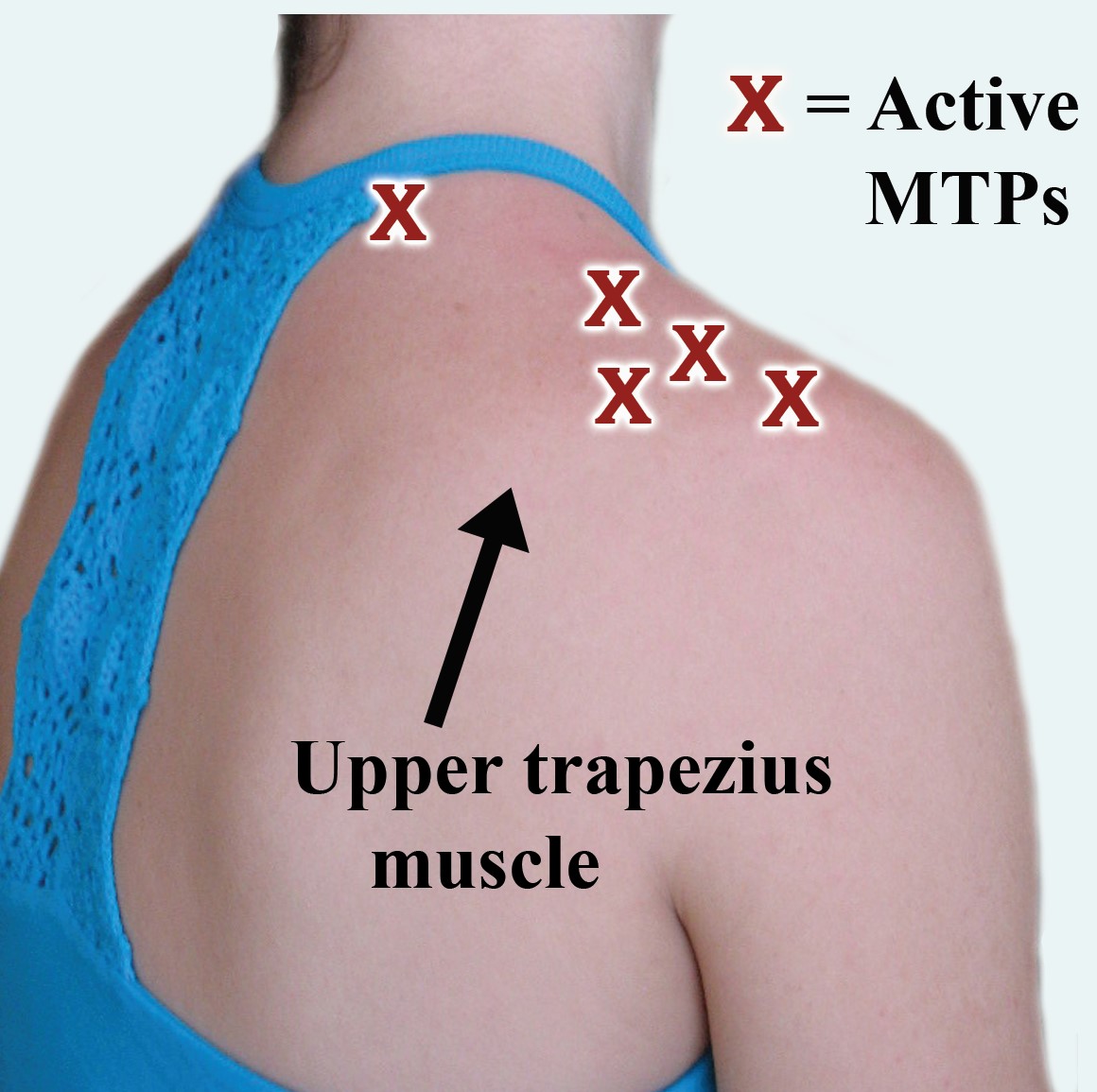
Ge sought to determine how many MTPs might be present in the two trapezius muscles as another part of his AFSA-funded study.4 He used needle EMG to map out active MTPs (those that produced spontaneous pain) and latent MTPs (those that did not hurt unless pressed) in a group of 22 fibromyalgia patients and 22 healthy subjects.
The average fibromyalgia patient had almost five active MTPs and four latents on each side of the trapezius muscle. The healthy subjects did not have any active but had five latent MTPs in the same muscle region. The pain pattern produced by the MTPs (active and latent) in fibromyalgia patients covered the head, neck, shoulders, mid and lower back, upper chest, and arms. In other words, your trapezius muscles are contributing to the brunt of your upper body pain.
Bottom line: Treating the MTPs in your upper trapezius muscle is a good place to start. You also need to be careful about not over straining your shoulder muscles because they are already overloaded with MTPs (minimize leaning your head forward).
1. Ge HY, et al. J Pain 11(7):644-651, 2010. AFSA-funded Study Article
2. Sikdar S, et al. Arch Phys Med Rehabil 90:1829-38, 2009.
3. Shah JP, et al. Arch Phys Med Rehabil 89(1):16-23, 2008.
4. Ge HY, et al. PAIN 147(1-3):233-40, 2009. AFSA-funded Study Abstract
