Projects Funded
Role of Neutrophils in Fibromyalgia
Principal Investigator: Shafaq Sikandar, Ph.D.
Queen Mary University of London, United Kingdom
Neutrophils are the first immune cells on the scene to attack foreign pathogens. They also signal other immune cells to help, but what does this have to do with your fibromyalgia symptoms? A prior study by Sikandar shows that injecting neutrophils from fibromyalgia patients into mice quickly produces chronic widespread pain in the mice. This reaction doesn’t occur with neutrophils from pain-free subjects.
Naturally, you want your neutrophils to respond to infections. However, it’s not healthy if they are activated when nothing is threatening your body. “The neutrophils from fibromyalgia patients appear primed to respond to something that isn’t there,” says Sikandar. “It’s almost like their programming is altered.” This AFSA-funded study explores how fibromyalgia neutrophils might be different and whether specific characteristics can be used as a blood marker.
Painful Impact
Neutrophils do not ordinarily produce widespread pain, so what are these cells doing in the mice to cause pain? Neutrophils from fibromyalgia patients invaded the dorsal root ganglia in the mice. These ganglia are the bulb-shaped structures that house the cell bodies (the nucleus) of the neurons. They reside just outside the spinal cord.
Alterations to the ganglia can magnify the sensory signals of neurons entering the cord. Indeed, the spinal cord neurons in mice injected with neutrophils from fibromyalgia patients become hyper-responsive to pressure within one hour.1 Both the pain thresholds and spinal cord neurons remain unchanged in mice injected with neutrophils from healthy people.
“It is counterintuitive to think that neutrophils are bad guys,” says Sikandar, especially given their protective role against infections. “But there is evidence in the literature to suggest otherwise.” Neutrophils don’t normally reside in the dorsal root ganglia either, yet those taken from fibromyalgia patients find their way there (at least in mice). Unfortunately, rodent experiments can’t explain why your neutrophils behave differently from people without pain.
Do fibromyalgia patients have more circulating neutrophils and are they in an activated state? And what about their programming, is it different? Sikandar’s study attempts to answer these questions and correlate the findings with fibromyalgia symptoms. But before diving into the specifics of this study, it’s important to understand how neutrophils typically operate.
A Neutrophil’s Life
Normally, neutrophils float around in the bloodstream in a neutral state (i.e., not activated). However, if there is a sign of infection or injury, they become activated and infiltrate the affected tissue. Once activated, they form neutrophil extracellular traps (NETs) to engulf the pathogen.2 NETs are weblike structures to trap the invader and their formation is called NETosis.
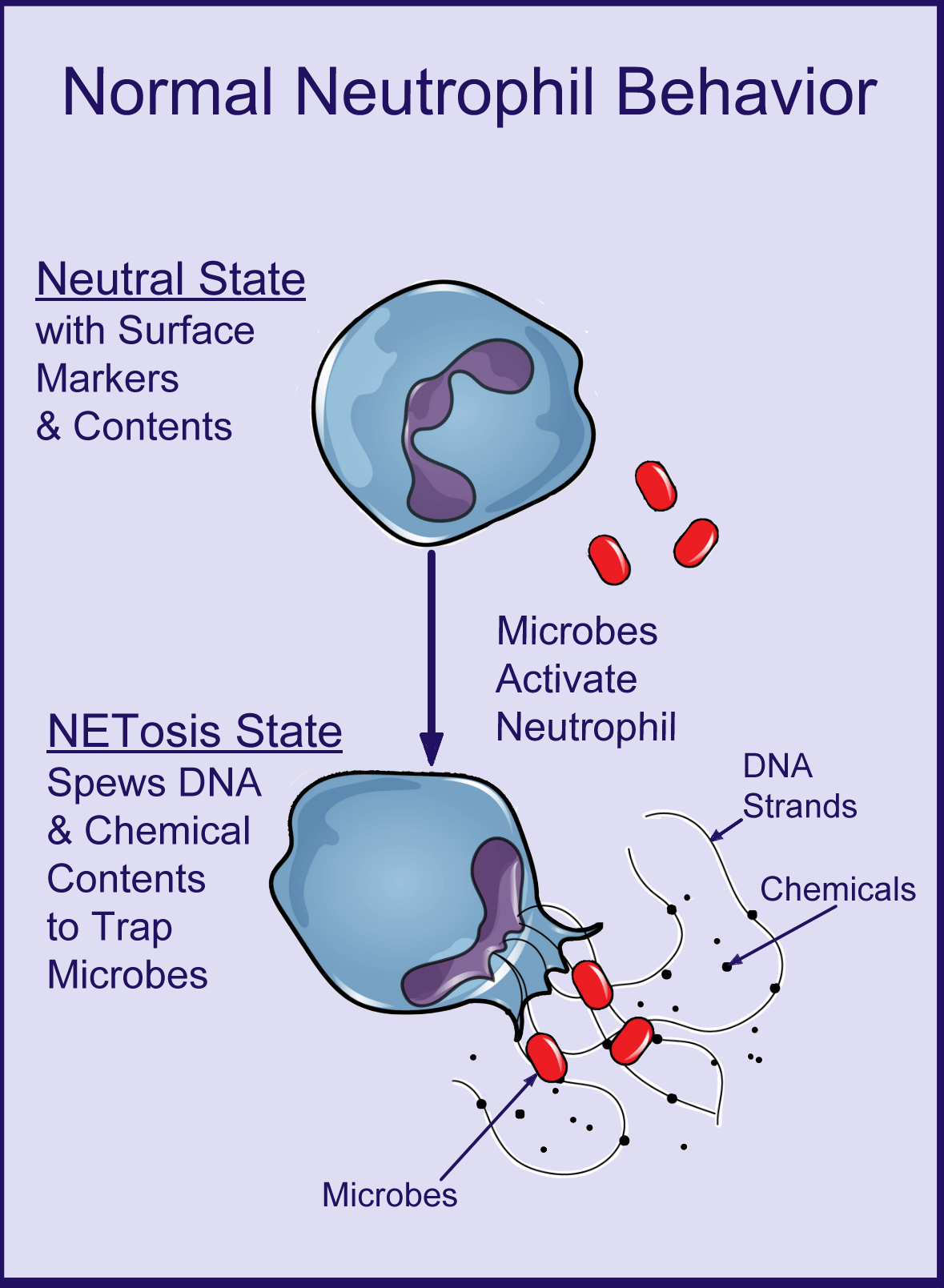
The surface markers on neutrophils are protein molecules that help the cell communicate with other cells. They tell a lot about their characteristics and how the cell is programmed to behave. For example, some markers help the neutrophil recruit other immune cells to the site of infection and others help the neutrophil move into specific types of tissues.
The surface markers reveal important information about the characteristics of a person’s neutrophils, but more is learned by assaying its contents. During the process of NETosis, the neutrophil spews out DNA and a variety of substances to neutralize the threat. All these substances communicate with surrounding cells (including neurons), so analyzing the contents is essential for fully understanding a neutrophil’s behavior.
Number & NETosis
A routine blood test measures your neutrophil cell count. Based on Sikandar’s preliminary data, “There seems to be more neutrophils in circulation in people with fibromyalgia.” Infections, inflammation, vigorous activity, and other situations can increase neutrophil counts. But generally, a higher number doesn’t cause symptoms.
Sikandar’s preliminary data also shows an increased degree of NETosis in fibromyalgia patients. “We need to see if there is an association with higher neutrophil numbers and NETosis,” says Sikandar. In addition, she will correlate this data with pain sensory testing and the severity of other fibromyalgia symptoms.
Looking at the activation state of neutrophils is commonplace in many diseases. But there was no reason to investigate them in fibromyalgia until Sikandar’s neutrophil experiment in mice. That was a turning point. Now there is ample cause to investigate these cells in fibromyalgia and compare the data obtained from healthy subjects
Surface Markers
Sikandar is using flow cytometry to measure neutrophil surface markers in fibromyalgia patients and healthy controls. “It’s a standard technique to study how immune cells change their characteristics (or phenotype) in different diseases,” says Sikandar. She adds that the role of many surface protein markers is known in both healthy and diseased states.
“Ideally we want to determine if the pattern of surface marker expression is different in fibromyalgia neutrophils,” says Sikandar. “If we know what the surface markers are, it might tell us why the neutrophils infiltrate the dorsal root ganglia in mice. It might also explain what drives the sensitization of neurons in the mice (and possibly fibromyalgia patients) to cause pain.”
“This part of the project might give us a mechanism of the disease,” says Sikandar. “But it might also give us a biomarker.” If the surface marker proteins are unique, they can serve as a fibromyalgia signature.
“There are two aspects to this part of the study,” says Sikandar. “The goal is to better understand neutrophil behavior in fibromyalgia and get closer to a peripheral circulating biomarker.”
Neutrophil Contents
To measure the neutrophil contents, you must break up the cells and run them through a mass spectrometry machine. The surface proteins can tell a lot, but the mechanism responsible for driving the pain and other symptoms may depend upon what’s inside the neutrophils.
Do the surface markers communicate with the neurons in the dorsal root ganglia to ramp up pain? Or do the contents released by the neutrophils communicate with the neurons? Given that the neutrophils from fibromyalgia patients (but not the controls) invaded the ganglia in the mice, the surface markers that control tissue movement are likely different. Still, it’s essential to capture the whole picture of what makes the fibromyalgia neutrophil tick.
Project Goals
Do various measures of pain and other fibromyalgia symptoms correlate with the activation state of neutrophils (i.e., NETosis)? “We know neutrophils from fibromyalgia patients can sensitize the neurons in mice,” says Sikandar. “And it’s logical to infer that if the neurons respond differently, then the neutrophils are also different. Yet we still need to show how the cells are altered, which is the main goal of this project.”
Another objective is to determine if neutrophils can provide a tangible biomarker. Examining the surface markers and the cellular contents will pin down specific characteristics, perhaps a fibromyalgia neutrophil phenotype. This is one possibility.
The NETosis findings might also provide a potential biomarker. For example, if the degree of NETosis correlates to pain sensitivity measures in patients, then the activation state of neutrophils can be a fibromyalgia biomarker.
What else are neutrophils doing besides driving pain hypersensitivity? Can changes in these cells be linked to other common symptoms such as fatigue, sleep disorder, or cognitive fog?
Finally, it’s important to know if specific neutrophil characteristics can be identified in two different fibromyalgia populations. Patients living in the United Kingdom will be compared to those living in Israel. If an abnormality exists in some patients but not others, it enables researchers to investigate what makes patients different. Also, an ongoing AFSA study involving the Israeli group is evaluating changes in gut bacteria. It’s possible that neutrophil function influences the gut or vice versa.
Research holds the key to better treatments. AFSA funded six projects in the past two years. Help us keep the momentum going!
Stay Current on Treatments & Research News: Sign up for a Free Membership today.
Dorsal Ganglia in Fibro | Increased Infection Rate | What is Fibro? | Why So Many Symptoms
References for Neutrophils & Fibromyalgia
- Caxaria S, Sikandar S, et al. PNAS 120(17):e2211631120, 2023. Free Report
- Maier-Begandt D, et al. Nephrol Dial Transplant 39(10):1551-1564, 2024. Free Report
