Possible Causes
Chaos in the Brain
![]()
The spinal cord and brainstem’s failure to put a lid on your pain means that more signals travel up to your brain. Over time, this leads to changes in brain chemicals as well as alterations in fibromyalgia brain function. Ordinarily, the brain operates in an efficient and coordinated fashion, but not so in people with fibromyalgia. In fact, your dysfunctional and chatterbox ridden brain likely contributes to problems with cognition, sleep control, hormone regulation, and other functions.
Noisy & Uncoordinated
Brain areas responsible for specific tasks should be in constant communication (i.e., connected) to produce a coordinated effort. For example, structures in the pain inhibitory network should be connected to one another to provide a united front. If your mind is wandering or asleep, a large “default” network linking internal thought processes will be activated. Conversely, the default network rapidly shifts to the background during mental tasks because the cognitive network is engaged.
In people with fibromyalgia, the pain inhibitory centers aren’t talking to one another, yet those known to enhance pain are chatting away. It’s as though your brain’s organization is more focused on making you hurt more, not less. In addition, your brain should be shouting to the brainstem to reduce the signals traveling up the cord, but instead its communication is more like a whisper. And the default network seems chronically turned on, which might explain your cognitive impairments and quasi-sleep state.
Could it be that your fibromyalgia brain is functioning under the false impression that there is a serious injury or an infectious threat to the body? It seems to be acting that way because the brain is not trying to reduce the incoming signals.
Lack of a coordinated effort between brain centers is just one of your many problems. Glutamate, which is toxic to the neurons, tends to accumulate in several regions. Conversely, GABA, which minimizes pain-related transmissions, is low in various brain areas. In addition, metabolic byproducts are high in various structures. Overall, the chemical imbalances reflect overworked brain centers that can’t keep pace with the pain processing demands.
Key Brain Centers
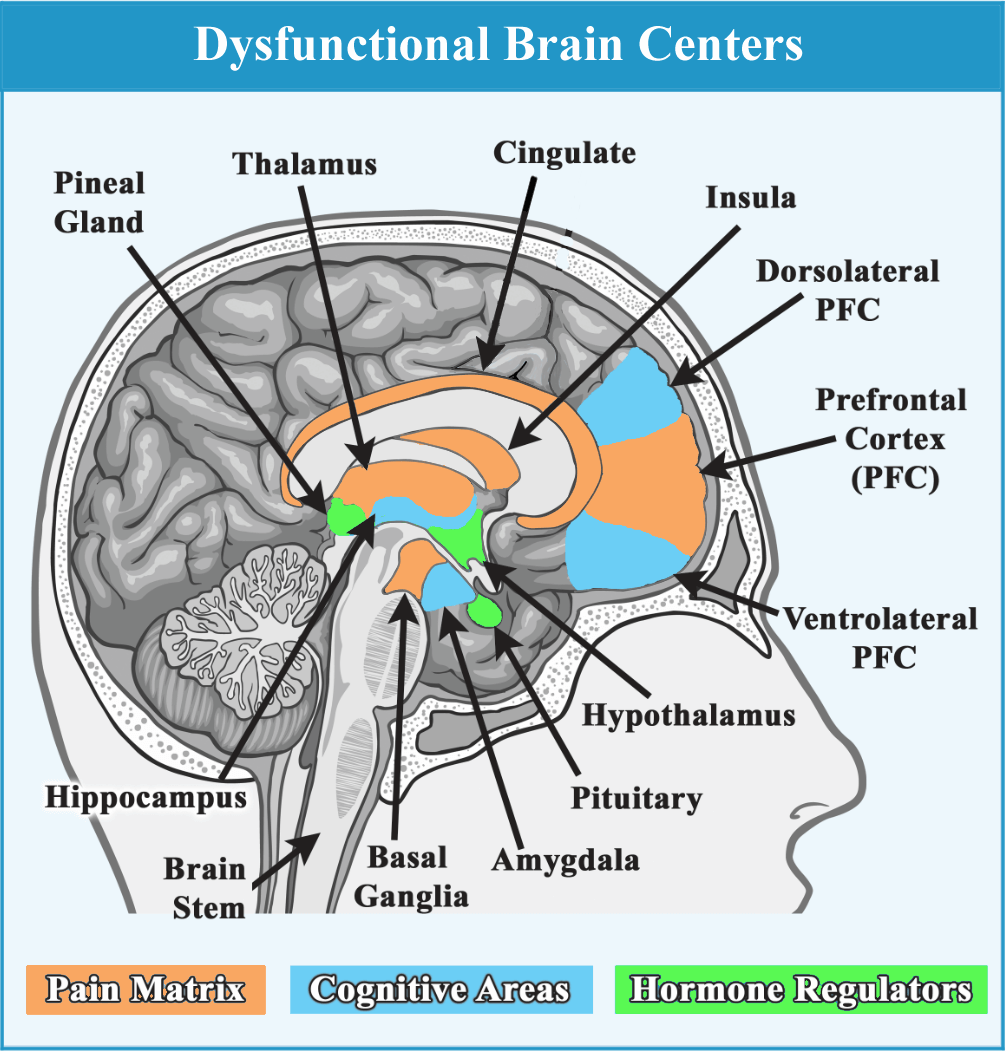
A few brain abnormalities are described below to illustrate how dysfunctional the brain is in people with fibromyalgia. The following diagram shows where the key brain structures are located. Ordinarily, brain centers should be able to multitask and pick up the slack of neighboring regions. But with so many areas overworked, your brain lacks the necessary flexibility to respond to challenges of any type (cognitive, painful or stressful).
Thalamus
Pain-related transmissions that sail through the brainstem, usually arrive at the thalamus. It’s located at the center of the brain and operates as a conduit for all pain-related input before being interpreted by the cortex. Unfortunately, the thalamus doesn’t properly distribute the load with other pain-processing centers. An abundance of glutamate and an imbalance of metabolic products in the thalamus is associated with higher pain scores in fibromyalgia patients.
Hypothalamus
This structure is next door to the thalamus and plays a key role in regulating many of the body’s hormones. The hypothalamus in fibromyalgia patients secretes two times the normal amount of corticotropin releasing hormone or CRH, a stress hormone that can lead to a suppressed immune system. Elevated CRH will eventually cause depressed mood and increased anxiety.
Prefrontal Cortex (PFC)
The mid-section of the PFC is a key player in processing pain, while its top and bottom regions are essential for cognitive functions (memory and concentration). An accumulation of glutamate impairs the function of this brain structure to shut down pain in fibromyalgia patients. It may also reduce working memory needed for multitasking and word finding.
Amygdala
How frustrated or anxious you are by your pain may be related to the function of your amygdala. Not only is glutamate higher in this structure, so are various chemical byproducts that are supposed to be cleared from healthy functioning brain cells. With the PFC not working properly, this causes your amygdala to unleash emotions, and it worsens one’s perception of pain. Loss of sleep further rocks the boat and makes you feel like you are riding an emotional roller coaster.
Cingulate
Pain is never pleasant, but this brain structure can modulate feelings of unpleasantness and sadness about one’s pain. The cingulate is part of the Top-Down pain inhibitory system, but it also plays a role in planning and motivation. Glutamate is high and dopamine is low, tipping the scales toward more pain, depressed mood, and loss of drive.
Insula
When inputs from the body or sensory info from the environment arrive at the insula (deep in the brain), it prioritizes the signals. In people with fibromyalgia, this structure is hyper-responsive to pain and all types of sensory inputs. This may explain your enhanced sensory sensitivities to sound, taste, odors, and bright lights. The insula appears to be lumping all inputs together and magnifying them.
Aside from causing sensory overload, the insula might be contributing to cognitive dysfunction (commonly referred to as fibrofog). Chronic activation of the insula in fibromyalgia patients is strongly tied to the activation of the default network, which promotes an “out to lunch” brain state. In healthy, pain-free people, the insula and the default network are divorced from one another … as they should be.
What is the evidence that the insula is tied to pain in fibromyalgia? In general, the greater the glutamate concentration in the insula, the greater the reduction in pain thresholds. This is a correlation that exists in all people (with or without fibromyalgia) because of the insula’s role in determining the significance of stimuli entering the brain. However, glutamate levels are much higher in fibromyalgia patients (plus GABA is low), so pain thresholds are half that of healthy controls.
Hippocampus
The most crucial brain structure for memory and learning is the hippocampus. Research in fibromyalgia patients shows this brain center is full of metabolic waste products, impairing its ability to function properly.
The hippocampus does more than help you think. It also tones down your body’s response to stress and plays a role in processing pain-related transmissions. This brain structure strongly relies on dopamine to communicate its actions with other brain areas and body systems. However, deficient dopamine levels could be crippling your hippocampus’ function.
Therapies to Quiet the Brain
Medications that simultaneously increase serotonin and norepinephrine (duloxetine, Savella, cyclobenzaprine, amitriptyline, and tramadol) can improve pain inhibition. The same holds true for medications that increase GABA (such as gabapentin and pregabalin). Reducing dietary glutamate may also help.
A variety of nondrug or alternative treatments will also tone down the sensory inputs that scramble your brain. Examples include TENS and CES devices, but you have many options. In addition, you can try different mind-body therapies (such as yoga), which are discussed in Fibro Friendly Exercises. Other approaches are described in Fibromyalgia Basics.
Stay current on Treatments & Research News with a FREE Membership.
Back To Brainstem; Next To Dopamine Link
