Fibromyalgia Basics
Pregabalin for Fibromyalgia
Reducing the Side Effects
![]()
Pregabalin (Lyrica) treats fibromyalgia pain and it also helps with sleep. However, most physicians follow dosing guidelines that assume every patient is the same. But fibromyalgia patients require a tailored approach to maximize pregabalin’s benefits while sidestepping unwanted side effects (such as weight gain and daytime sedation). So, here is what you need to know:
- Physicians commonly prescribe the drug because it is FDA-approved for treating fibromyalgia pain.1
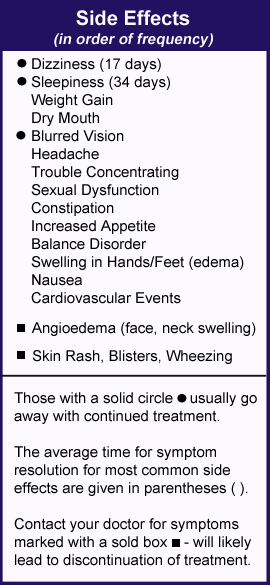
- Many side effects go away after two to four weeks while some are deal breakers.
- Reducing dose and switching to nighttime use only are two strategies to minimize side effects.
- Taking lower doses of 25 to 75 mg of pregabalin throughout the day provides symptom benefits for many patients.
If you try pregabalin, it’s important to be aware of the side effects. You also need to be proactive about discussing dosing changes with your doctor. To help you out, several physicians offer their advice.
Effectiveness for Fibro
Pregabalin relieves fibromyalgia pain by boosting your central nervous system production of GABA. This transmitter is important for your pain fighting system and it also aids with sleep. GABA is low in people with fibromyalgia, so pregabalin ought to help.
But what are the odds that this drug can cut your pain by more than 30 percent? That’s a tall order and the answer is only 1 out of 10, mostly because patients encounter unwanted side effects.2
Given the low odds that pregabalin will effectively treat your fibromyalgia, why bother with it? Patient response varies tremendously and there is no way to predict who will respond with “I got my life back.”
One more point: the recommended pregabalin dosing for fibromyalgia patients starts at 75 mg twice a day for the first week. Next, patients are supposed to jump to 300 mg/day and possibly go to 450 mg/day by the third week. This is too aggressive and the high pregabalin dosage is bound to trigger side effects in most fibromyalgia patients. Yet settling on a lower dose can offer pain relief and improve sleep.
Common Side Effects
For the most part, pregabalin’s side effects are dose dependent. The more you take, the greater your chances of getting a particular side effect.3
“The most common reasons for discontinuing pregabalin are sleepiness and weight gain,” says Kenneth Miller, M.D., of Danbury, CT. “Blurred vision occurs in less than 10 percent of patients and usually resolves with time.” If you encounter this problem, notify your doctor because you need to have routine eye exams. “Dry mouth and constipation occur more often at the higher doses,” adds Miller.
Weight gain can plateau after four months on pregabalin or it can take two months for this side effect to occur.4 The average weight gain per month for patients at the 300 mg/day dose could be as high as 4.5 percent of a person’s body weight. “I have seen patients gain 10-15 pounds during the first 3-4 months,” says Miller. “If a patient gains more than this, I advise discontinuing the drug. Pregabalin increases appetite, so monitor your caloric intake and increase physical activity.”
“Patients who retain fluids (edema) can take a mild diuretic,” says Miller. In fact, Lesley Arnold, M.D., of Cincinnati, OH, says she starts patients with an over-the-counter diuretic, such as pamabrom, but she gets mixed results. “It’s the active ingredient in the PMS drugs and is sold in the diet section of drugstores,” says Arnold. “If you have a good response to pregabalin but the fluid retention is uncomfortable, give diuretics a try.”
Sexual dysfunction occurs within weeks of using pregabalin.5 Neither erectile dysfunction nor loss of libido is dose related and they resolve with discontinuation. Cardiovascular events (deep vein thrombosis and pulmonary embolism) also occur more frequently in fibromyalgia patients taking pregabalin.6
Nighttime Dosing
I. Jon Russell, M.D., Ph.D., of San Antonio, TX, suggests that patients take pregabalin at bedtime to minimize dizziness. Indeed, nighttime dosing of pregabalin improves the quality of sleep in fibromyalgia patients.7
The drug also reduces the production of pain-promoting and sleep-disrupting immune substances (cytokines). And it does so at the low dose of only 150 mg/day.8
But will taking pregabalin only at night provide enough daytime pain relief? “There is a 50 percent chance that this strategy will be effective,” says Kevin Hackshaw, M.D., now at the University of Texas in Austin. He adds that predominant nighttime dosing leads to less daytime side effects for the other problems listed in the table.
Using this strategy, blurry vision and dry mouth shouldn’t bother you during sleep. Also, edema (especially swelling in the legs) is reduced because you are not on your feet when the higher dose of the drug is in your system. Taking the brunt of pregabalin at night gives your GI system a break from the drug during the day. This reduces constipation issues.
Even if you find nightly dosing of pregabalin helpful, Hackshaw says, “It is more often effective for fibromyalgia as an all-day medication.” So, Hackshaw offers a tailored dosing strategy to help you get around the daytime side effects of pregabalin.
Tailored Approach
To achieve daytime pain relief, Hackshaw places patients on 25 mg in the morning and 25 mg in the late afternoon. Then patients take anywhere from 100 to 150 mg at bedtime. “You don’t have to take the 150 mg dosage two times a day to get relief from pregabalin.”
Sometimes Hackshaw writes two prescriptions, one for 25 mg capsules of pregabalin to be taken twice daily, and a separate script for 150 mg capsules to be taken at bedtime. This method may be the most convenient for patients and is usually covered by insurance companies, but it requires patients to pay for two copays. This approach is more costly, but now that pregabalin is available as a generic, it may be doable.
“A way to get around the issue of two copays is to write just one prescription for 25 mg caps,” says Hackshaw. “For example, I write the script for one 25 mg cap in the morning, one 25 mg cap in the afternoon, and six 25 mg caps at bedtime. Insurance companies usually approve prescriptions written this way and there is only one copay.”
Taking the brunt of pregabalin at bedtime with small booster doses during the day, is bound to minimize side effects. It also makes sense to increase nighttime dosing to improve sleep. So, why is this pregabalin dosing method for fibromyalgia not publicized? Drug manufacturers must recommend the FDA-approved dosing schedules (e.g., 150 to 225 mg twice daily).
Real World Dosing
If you tried pregabalin but the side effects prevented you from reaching the recommended daily dose of 300 to 450 mg, you are a typical fibromyalgia patient.
Out of 126 fibromyalgia patients in a clinical practice, 113 were able to tolerate pregabalin.9 However, the average dose was only 150 mg/day or 75 mg of pregabalin twice daily.
The point is, higher doses generally don’t offer more benefits; just more side effects.
- To learn about other medication options, see Medications.
- If you are curious about nondrug approaches, see Alternative Therapies.
Symptoms | What Is Fibro | Finding Doctor | Muscle Pain Relief | Fibro Friendly Exercises
AFSA funded six projects in the past two years. Help us fund more next year.
Get free treatment help delivered to your inbox when you join AFSA. We interview the experts and compile patient-friendly articles. All we need is your name and email.
References for Fibromyalgia Pregabalin
- Rico-Villademoros F, et al. Clin Exp Rheum 38(Suppl 123):S72-S78, 2020. Free Report
- Donnelly L, et al. Am Fam Physician 97(9):online, 2018. Free Report
- Mease PJ, et al. J Rheumatol, 35(3):502-14, 2008. Abstract
- Arnold LM, et al. Postgrad Med 129(8):921-933, 2017. Abstract.
- Hamed SA. Clin Neuropharmacol 41(4):116-122, 2018. Abstract
- Pan Y, et al. PLOS ONE 19(7):e0307515, 2024. Free Report
- Roth T, et al. Clin J Pain 32(4):308-12, 2016. Abstract
- Ellergezen P, et al. Arch Rheumatol 38(2):307-314, 2023. Free Report
- Arkfeld DG, et al. American College of Rheumatology Meeting San Francisco, 2008.
