Projects Funded
Tender Points are Mostly Treatable MTPs
The rock-like nodules in your muscles are major pain generators that can be treated. In fact, 90 percent of the tender areas that physicians initially used to diagnose fibromyalgia are myofascial trigger points or MTPs. Studies by Hong-You Ge, M.D., Ph.D., and Cesar Fernandez-de-las-Penas, Ph.D., both found that the more MTPs you have, the greater your overall pain. Learn why this is the case and how you can treat the trigger points in your back to relieve fibromyalgia pain.
Fibromyalgia
The Mirror Image of Normal?

Tired of being told you look fine or frustrated that your lab tests fail to document your pain? Rest assured, there is something going on beneath the surface that causes you grief but leaves you looking normal.
Studies by both researchers identify an important distinction in the muscles between healthy pain-free people and fibromyalgia patients. It has to do with myofascial trigger points (MTPs), the areas that hurt and radiate pain in fibromyalgia patients. However, the explanation is not what you might think. Most everyone has MTPs—even people who don’t have pain—but yours are different.
Turned On
The presence of MTPs in your achy muscles doesn’t distinguish you from healthy people, according to Hong-You Ge, M.D., Ph.D., of Denmark. He found 11 MTPs (on average) in a group of fibromyalgia patients and a similar number in pain-free controls.1 Ge also discovered that the MTPs occurred more commonly in the same areas of the musculature. Yet there is one major difference: the state of the MTPs.
Your MTPs are turned on (they are active), while everyone else’s are in a dormant state (they are latent). Even if you try to relax, your active MTPs generate pain. No one needs to press on the areas for them to hurt. In healthy people (pain-free), their latent MTPs are not turned on, so they don’t produce any discomfort.
MTPs occur in muscle areas that are prone to being overused. The strain causes a sustained contraction of the muscle fibers (they become bunched up), forming a firm nodule. People are seldom aware of latent MTPs because they don’t hurt. On the other hand, active MTPs are more evolved and possess additional characteristics.2
- Hurt all the time (even when they are not pressed)
- Contain a reservoir of chemicals that irritate nerve endings
- Restrict blood flow (making it harder to use the muscle)
- Radiate significantly more pain than latents when pressed
Reflections of Pain
If latent MTPs don’t cause pain, how did Ge locate them in healthy people in the first place? He mapped the active MTP locations he found on the fibromyalgia patients onto healthy height-weight-matched controls. It’s somewhat like reflections in a mirror, which enabled Ge to examine these regions for the painless nodules known as latent MTPs.
Fibromyalgia patients know where they hurt, so Ge used their pain drawings to guide his search for MTPs.3 Then he examined the areas to zero in on active MTPs (the firm knots that radiate pain when pressed).
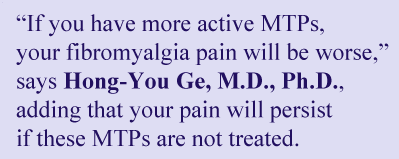
Forty areas for potential MTPs, 20 on each side in a symmetrical pattern, were identified by the fibromyalgia patients. On average, each fibromyalgia patient had 11 active MTPs. The most common locations are illustrated.
When Ge examined the control subjects, he did not find any active MTPs, only 11 latents. Ironically, the latent locations mirrored what Ge found for the active MTPs in the fibromyalgia group.
Symmetry
The number of key active MTPs on the right side of the body for fibromyalgia patients appears to match those found on the left side. Why the symmetry?
“This is likely due to dual activation of the muscle groups for performing most physical activities,” Ge says. “Or it could be caused by the spreading of pain from one side of the spinal cord to the other. Either way, this is an important clue when identifying and treating trigger points in people with fibromyalgia.” For example, if an active MTP exists in your right forearm below the elbow, check the other arm!
More Active MTPs
Greater Pain
The greater number of active trigger points, the greater the pain severity in people with fibromyalgia. Both Ge and Cesar Fernandez-de-las-Penas, P.T., Ph.D., of Spain, identified this correlation between MTPs and pain.4 So, if you have more active MTPs, your fibromyalgia pain will be worse. That’s why it is essential to learn how to identify and treat them.
Fernandez-de-las-Penas found that “the higher the number of active MTPs, the lower the pressure pain threshold levels.” In other words, your body’s ability to detect pain is greatly enhanced when thresholds are lower. This finding is no surprise given that active MTPs contain pain-sensitizing chemicals that irritate nerve endings.
Like Ge, Fernandez-de-las-Penas found an average of 10 active MTPs in his fibromyalgia group. He also only detected latents in the healthy subjects.
Fibromyalgia Reproduction
How much of your fibromyalgia pain is caused by active trigger points? Both Ge and Fernandez-de-las-Penas addressed this question. Each time they pressed on an active MTP, patients shaded the areas that hurt on a body diagram. A composite pain drawing representing all the active MTPs was generated for each patient. The same was done for the latent MTPs in the healthy group, which only produced a negligible amount of discomfort.
“The local and referred pain elicited from widespread active MTPs fully reproduced the overall spontaneous fibromyalgia pain pattern,” says Fernandez-de-las-Penas. Ge’s research produced the same results. In other words, your tender areas or active trigger points play a major role in generating your body-wide fibromyalgia pain pattern.
Treatment Approach
Identifying active MTPs improves your treatment success. “If these active MTPs in the muscles are not treated, fibromyalgia pain will persist.” Ge suggests that “pain drawings be used as an aid for locating active MTPs.”
Pain drawings identify your most intense regions of discomfort. They can serve as a tool to help your provider prioritize which areas to treat first. However, an understanding of the referred pain patterns produced by MTPs is helpful. For example, Ge comments that an MTP in a back shoulder muscle will likely shoot pain to the front of the shoulder. So, you need a provider to interpret your drawings.
Physical therapists and deep-tissue massage experts often possess the talent needed for treating MTPs. Some physicians, particularly physical medicine specialists or physiatrists, are also skilled in this area. If you don’t have an MTP treatment provider, you can learn to reduce these painful areas yourself. For step-by-step guidance, see the section on Muscle Pain Relief.
Learning to treat MTPs takes a little time but is worth the effort. Research shows that deactivating one active MTP leads to a reduction in overall fibromyalgia pain. Just think of the benefits you can reap by treating several of your active MTPs?
Spotlight on Back Pain
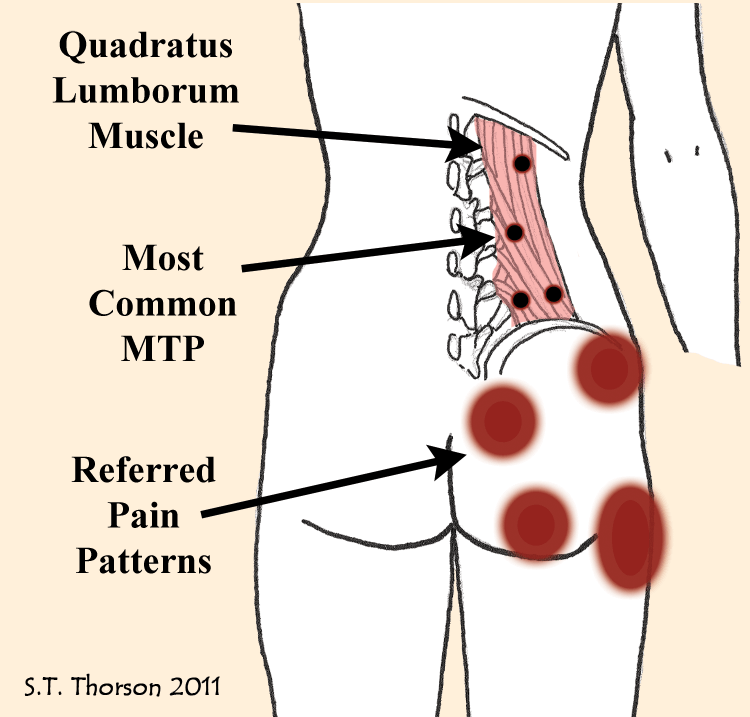
Ge discovered that the most common fibromyalgia trigger points are not even included in the old tender point exam. In particular, the quadratus lumborum in the low back contains the highest incidence of MTPs (72 percent) in fibromyalgia. This is also the most common muscle for latent MTPs in healthy people.
The quadratus lumborum attaches at the back ridge of your pelvic bone and fans out into multiple sections, each one attaching to a different level of the vertebrae in your low back or lumbar region. Active MTPs in this muscle are the primary source of low back pain and referred pain to the hips and gluteal muscles (e.g., buttocks) in people with fibromyalgia.
What are some of the signs that your quadratus lumborum might have an active MTP? The following actions will produce more pain: turning over in bed, standing upright, bending over to lift objects, and twisting the trunk. Getting out of a chair can also be agonizing if the quadratus lumborum contains an active MTP.
If you identify with the pain patterns in the diagram or the above movements aggravate your pain, get help. Your quadratus lumborum works all day to keep you upright. Active MTPs in this lower back muscle must be treated to prevent your fibromyalgia pain from spreading.
Get free treatment help delivered to your inbox when you join AFSA. We interview the experts and compile patient-friendly articles. All we need is your name and email.
For more info on MTPs and treatment methods, see our section on Muscle Pain Relief.
Symptoms | Medications | Alternative Therapies | Finding Physical Therapists | Exercise Difficulties
Fibromyalgia Tender & Trigger Point References
- Ge HY, et al. Arthritis Res Ther 13(2):R48, Mar 22, 2011. Free Article
- Pradeep A, et al. BMC Musculoskelet Disord 24(1):624, 2023. Free Article
- Ge HY, et al. J Pain 11(7):644-51, 2010. Free Article
- Alonso-Blanco C, Fernandez-de-las-Penas C, et al. Clin J Pain 27(5):405-13, 2011. Free Abstract
