Fibromyalgia Basics
Fibromyalgia Sleep Treatments

If you toss and turn all night, unable to catch a wink, you have insomnia. Granted, your brain processes are messed up and likely more complicated than a typical case of restlessness. Naturally, you just want to know what treatments can put an end to your fibromyalgia sleep difficulties. Yet you can’t overlook restless legs syndrome (RLS) and obstructive sleep apnea (OSA) because they warrant special treatment.
Thirty percent of fibromyalgia patients have RLS. People describe it as a relentless urge to move their legs to escape unpleasant sensations. If you relate to these symptoms, check our RLS treatment article. If you snore, you may have OSA. This disorder occurs in 15% of patients. It’s diagnosed by a sleep study and is often treated with CPAP.
Clinical trials in fibromyalgia focus on relieving the pain rather than treating the sleep disorder. Therefore, the data in this article pertains to studies in people with insomnia.
Preparing for Sleep
Medications alone won’t be enough if your sleeping environment isn’t comfortable and your body isn’t relaxed. Fibromyalgia patients sleep best with a soft bed (at least a 3-inch mattress topper or an additional under quilt) and plenty of supportive pillows.
“I recommend everyone try cognitive behavioral therapy for insomnia (CBT-I) before trying medications,” says Andrew Krystal, M.D., Ph.D., sleep researcher at the University of California-San Francisco. “Many people get benefit from CBT-I and, if it is helpful, it has essentially no side effect risks.”
The basic tenant of a CBT-I program is to get your body ready for sleep. Your doctor needs to refer you to a therapist and it takes time to learn. CBT-I is the first-line treatment for insomnia and will help you cope with your nighttime frustrations. It probably won’t be enough to treat the scrambled sleep of fibromyalgia, so medications are likely necessary.
Before examining your sleep treatment options, make sure you are not taking an alerting medication close to bedtime. Selective serotonin or norepinephrine reuptake inhibitors, such as fluoxetine, escitalopram, or Savella can interfere with sleep. Talk to your doctor about switching to less activating medications or taking them earlier in the day.
Insomnia Medications
“There is no one best medication for insomnia,” says Krystal. “The key is to choose the right medication for the type of sleep problems you are experiencing.” Is your primary concern falling asleep (sleep onset), staying asleep (sleep maintenance), or is it a combination of both? Also, do you have anxiety or depression? The answer to these questions helps guide medication choices.1,2
When trying a new treatment for sleep, Krystal says, “Typically, a week is sufficient.” If you fail to respond to usual insomnia therapy, he recommends getting a sleep study to look for other conditions like obstructive sleep apnea.
The sleep disorder in fibromyalgia is chronic, but you should know that many doctors believe insomnia medications should be limited to short-term use. This viewpoint is based on outdated recommendations by the American College of Physicians. It ignores the newer insomnia drugs shown to be effective for long durations.
An expert panel of seven sleep researchers evaluated the data on the newer insomnia medications and disagreed with only using them for short-term use.3 Instead, they recommend that the appropriate duration needs to be individualized based on the balance of benefits and harms. This is especially important for older adults. Also, patients need to be evaluated on a regular basis.
Even if your doctor prescribes a sleep medication long term, your options may be limited. Many medications are scheduled IV substances (DORAs & Z-Drugs), which involve more prescriber oversight. As a result, the less regulated medications are addressed first.
Initial Options
Except for ramelteon, the sleep medications below are already used to treat fibromyalgia on a chronic basis. A small nightly dose may be worth a try.
Doxepin – This drug is used at low doses between 3 and 10 mg to selectively block histamine to help with sleep.4 At the low dose, doxepin does not cause dry mouth or the other common side effects of tricyclic antidepressants. “Clinically, if 6 mg is not strong enough,” says Krystal,” I increase the dose until either benefit or side effects occur. This occurs between 6 and 10 mg.” He starts people on the liquid version at 3 mg (1 mg for elderly) because it is easy to titrate. Doxepin is best for preventing early morning awakenings (sleep maintenance). If it doesn’t help with sleep onset, take it 90 minutes before bedtime so that blood levels peak when you slip into bed.
Ramelteon – This drug activates the melatonin receptor in your brain to help you fall asleep (i.e., sleep onset). If you struggle to get to sleep but don’t have much problem staying asleep, ramelteon could be a good choice for you. One downside is cost.
Pregabalin & Gabapentin – Pregabalin (25-200 mg) is sedating and can improve sleep. It can also treat anxiety, but often causes side effects, such as daytime sleepiness and weight gain. Despite being a scheduled V drug, pregabalin is approved for daily use in fibromyalgia patients. Gabapentin (600 mg) is a similar drug but is less sedating and it’s not scheduled.
Other Sedating Meds – Amitriptyline (10 mg) and cyclobenzaprine (10 mg) are sedating drugs often prescribed for fibromyalgia sleep. The effectiveness of these drugs is debatable but may be worth trying at the lowest possible dose.5 Otherwise, side effects can surface, such as hangover sedation and dry mouth.
DORAs
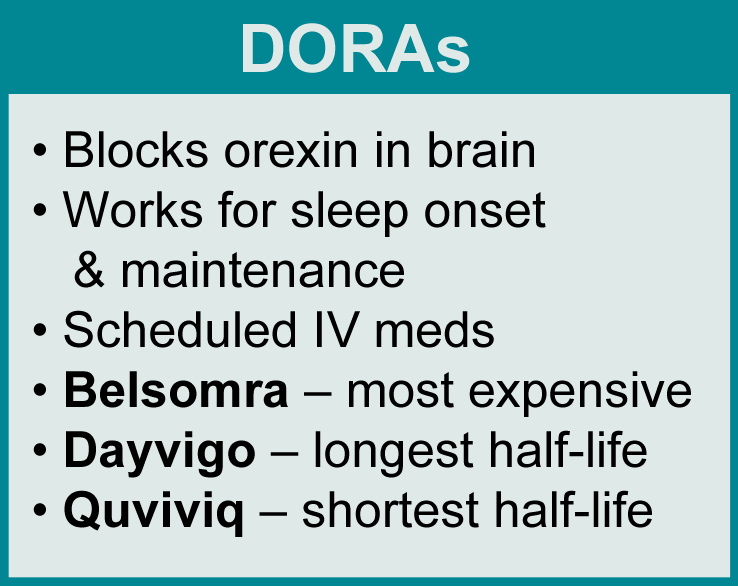
Orexin is a neurotransmitter that keeps you awake during the day. Blocking the release of this transmitter helps you fall asleep and stay asleep. This latest class of insomnia medications targets both orexin receptors in the brain, and they are called dual orexin receptor antagonists (DORAs).
There are three drugs in this class: suvorexant (Belsomra), lemborexant (Dayvigo), and daridorexant (Quviviq). No generics are available (making them more expensive), and prior authorization is often required by insurance companies. As a result, doctors must document that cheaper alternatives do not work.
The clinical trials for all three DORAs lasted a full year, showing they continue to work long term. Also, they have minimal blunting of arousal if you need to wake up and get moving in the middle of the night. But the most common side effect of DORAs is sleepiness.
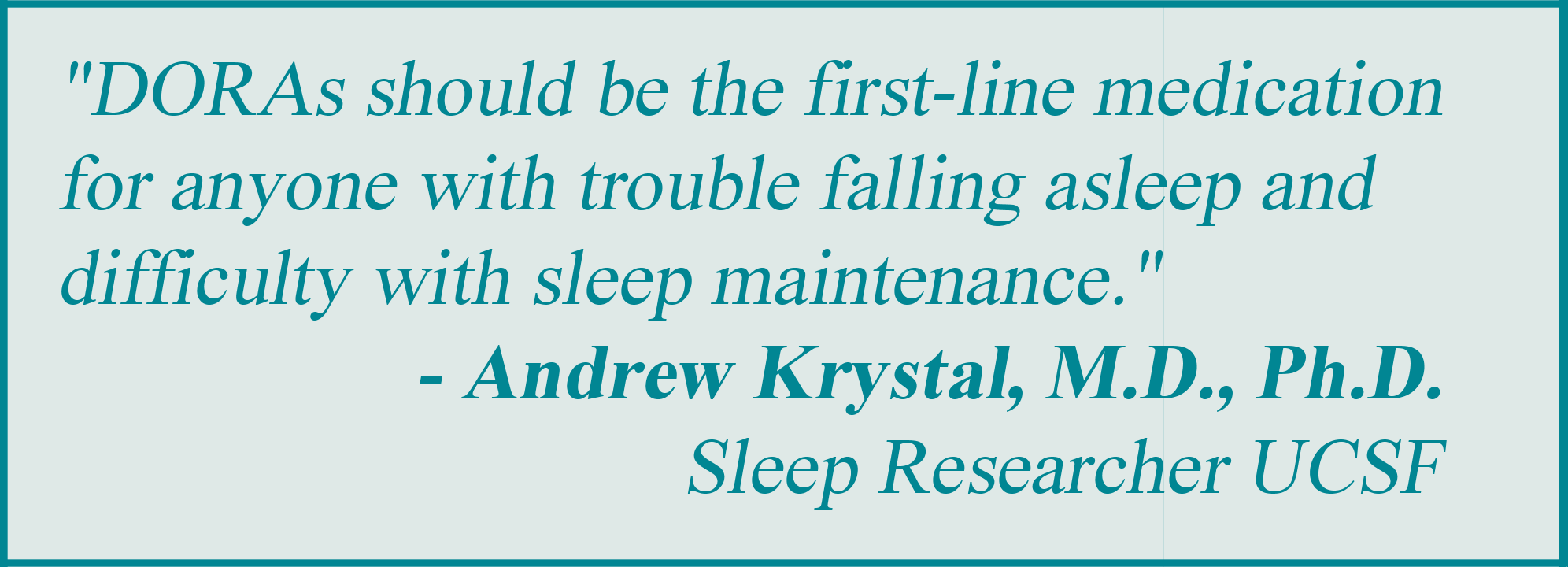
Unlike doxepin, DORAs exert robust effects on sleep onset, but they also have some abuse liability. “These agents should be the first-line medication for anyone with trouble falling asleep and difficulty with sleep maintenance,” says Krystal.
Belsomra – This was the first DORA FDA-approved for insomnia yet it is the most expensive one. Typical dose is 40 mg (30 mg for people over 65).
Dayvigo – The two available doses are 5 mg and 10 mg. Dayvigo has the longest half-life of the DORAs (18 hours), which could be a concern for next-day function.6
Quviviq – This DORA has the shortest half-life (8 hours), potentially making daytime side effects less risky. The two available doses are: 25 mg and 50 mg.
Impairments of psychomotor function are less likely with DORAs than the Z-drugs. However, fibromyalgia patients vary widely in their response to medications and the Z-drugs represent another sleep treatment option.
Z-Drugs
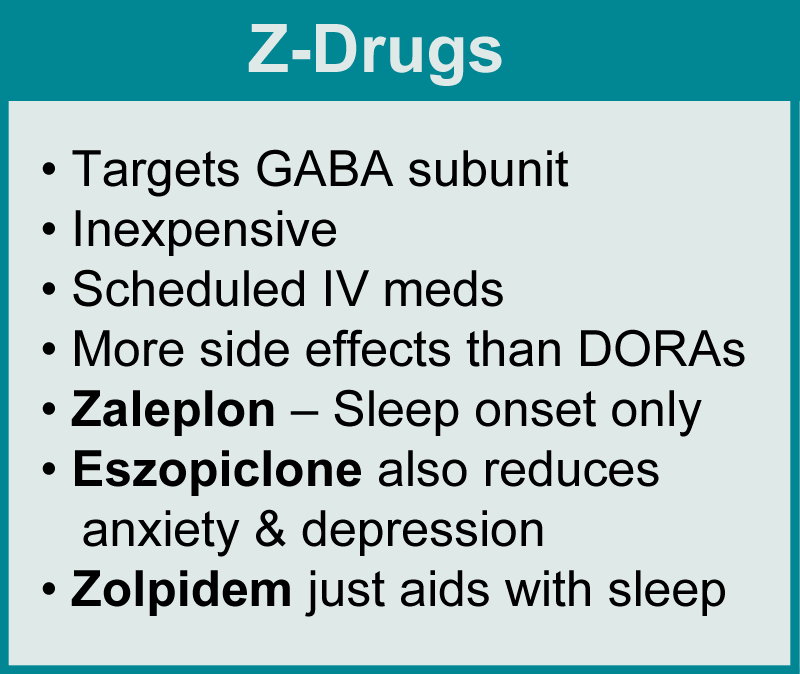
Zolpidem, zaleplon, and eszopiclone were developed as an alternative to benzodiazepines, and are referred to as the Z-drugs. While both drug classes target the GABA receptor, the Z-drugs more selectively work on a subunit that exerts a hypnotic effect. Unfortunately, the Z-drugs can also be abused and may impair psychomotor function (increasing risks of falls).
If you have exhausted all other options and you still can’t sleep, your doctor might consider a Z-drug. But keep in mind that prescription drug monitoring programs and state medical boards can be a deterrent to sympathetic doctors.
Zaleplon is very short-acting. It may put you to sleep but it won’t keep you there. This leaves zolpidem and eszopiclone as your two options.
“There are two clear benefits of eszopiclone over zolpidem,” says Krystal. “Eszopiclone lasts a bit longer so it can help more with sleep maintenance problems.” In addition, it doesn’t just work to treat insomnia, it also helps relieve depression and anxiety. Zolpidem only improves the insomnia.
Sleepwalking, and next-day drowsiness and dizziness are common side effects of the Z-drugs.7 Eszopiclone can also produce a bitter taste in the mouth in the morning but can be minimized with mints.
Future Sleep Options
Night after night of inability to sleep can make you feel like you are falling apart at the seams. Understandably, you want something that can put your brain to sleep without side effects and the baggage of scheduled drugs.
An alpha-stim (using CES) is a nondrug device FDA-approved for anxiety and insomnia, and an AFSA-funded study is examining its ability to treat your sleep. Unfortunately, insurance companies won’t pay for it. Ideally, the AFSA study will pave the way for expanded trials on the alpha-stim. This will provide insurance companies with the proof they need to cover the cost ($840).
The problem with CBT-I is access to providers. Krystal says two FDA-approved online prescription therapeutic programs show strong evidence for improving sleep. One is Somryst and the other is SleepbioRx. The barrier is insurance reimbursement. Some companies cover these programs and hopefully more will in the future. In the meantime, check with your insurance company about coverage.
If your insurance doesn’t cover these programs, there are websites that offer tips to improve your sleep. Check out CBT-I Coach (App- iOS/Android) and This Way Up Insomnia Program (Web).
Research holds the key to a better life. AFSA funded six projects in 2024 and 2025; help us fund more!
Don’t Miss a Beat on New Treatments & Research: Sign up for a Free Membership today.
Restless Legs | Medications | Treating Fatigue & Brain Fog | Mondrug Treatments | Lifestyle Changes
References for Fibro Sleep Treatments
- Krystal AD. J Sleep Res 32(6):e14084, 2023. Abstract
- Rosenberg RP, Krystal AD. Psychiatrist 82(6):E120008AHSC, 2021. Free Report
- Zee PC, et al. J Clin Med 12(4):1629, 2023. Free Report
- Fisher M, et al. Sleep Breathing 29(2):158, 2025. Free Report
- Pathak A, at al. Rheumatology 64(8):4495-4516, 2025. Free Report
- Leon-Barriera R, et al. Cleve Clinic J Med 92(1):43-50, 2025. Free Report
- Rosenberg RP, et al. Prim Care Companion CNS Disord 25(1):22nr03385. 2023. Free Report
