Infections in Fibromyalgia & Defective Immune Response
Treatment & Research News
Infections in Fibromyalgia
& Defective Immune Response
Home | Treatment & Research News
Feel like your body is a magnet to every infectious bug in the environment? A large population-based study involving 9,232 fibromyalgia patients and 46,160 controls confirms your suspicions.1 Regardless of the type of invader or the area of the body affected, the frequency of infections is higher in people with fibromyalgia and immune system studies shed light on this subject.
Infectious Disease Rates
Recent data shows fibromyalgia patients are slightly more likely to die of infections. Naturally, this begs the question: do infections occur more commonly in patients and if so, which types? Based on medical records spanning a ten-year period, the odds ratio for various infectious diseases were determined. An odds ratio (OR) of 1.0 means you do not have an increased risk of infection. However, an odds ratio of 2.0 means you are at double the risk for a particular infection.
“The fibromyalgia patients had significantly higher incidence of viral, bacterial, fungal, and parasitic diseases compared to the controls,” says Michal Vinker-Shuster, M.D. Here is a breakdown of the various infections by body region affected:
Respiratory Tract
- Upper respiratory tract infections (OR 1.5)
- Acute bronchitis (OR 1.5)
- Acute tracheobronchitis (OR 1.8)
- Acute bronchitis (OR 2.1)
- Influenza (OR 1.8)
- Sinusitis (OR 2.0)
- Otitis media (OR 1.8)
- Otitis externa (OR 1.5)
- Pneumonia (OR 1.6)
Gastrointestinal (GI) System
- pylori gastritis (OR 2.0)
- Candidal esophagitis (OR 7.9)
- Giardiasis (OR 3.4)
Genitourinary Infections
- Urinary tract (OR 1.8)
- Pelvic inflammatory disease (OR 3.2)
Skin & Soft Tissue (bacterial)
- Abscess (OR 1.7)
- Cellulitis (OR 1.6)
- Impetigo (OR 1.5)
Skin & Soft Tissue (fungal)
- Tinea pedis or fungal foot infection (OR 1.6)
- Tinea cruris or fungal groin infection (OR 1.7)
- Tinea versicolor or fungal skin infection (OR 1.9)
- Candidiasis or yeast infection (OR 2.0)
Fibromyalgia patients also exhibited higher rates of systemic viral infections such as cytomegaloviral (CMV) disease and COVID-19, in addition to bacterial infections such as staphylococcus. It should also be noted that another study showed increased rates of periodontitis disease in fibromyalgia patients, especially in young men.2 This gum disease is also known as gingivitis and is usually caused by a bacterial infection.
Possible Explanations
Due to the life-impacting symptoms of fibromyalgia, patients probably visit their doctor more often than healthy people. As a result, infections are more likely to be documented in your medical chart. However, it doesn’t explain the increased mortality rate in fibromyalgia due to infections. More than likely, your greater susceptibility to harmful pathogens stems from problems with your immune system defenses.
Natural Killer Cells
As their name implies, natural killer cells play a pivotal role in reducing viral replication and combating both bacterial and fungal infections. In fibromyalgia patients, these cells are persistently activated, yet their quantity in the blood is depleted.3 Although no one knows what triggers their activated state, exhausted natural killer cells provide a breeding ground that promotes infections.
Mast Cells
Your skin, mouth/nasopharynx, lungs, esophagus, and entire gastrointestinal (GI) tract are lined with mast cells. Your brain and blood vessels also contain mast cells. They are a ubiquitous immune cell that forms a protective barrier to reduce the odds that infections trespass into your system.
When mast cells detect a foreign substance, they pour out chemicals to increase blood flow and recruit other immune cells to the area. This includes histamine as well as inflammation-promoting substances such as the cytokines IL-1, IL-6, and TNF. Ideally, these activated mast cells help clear the pathogen from the area. But if chronically activated, they may not be doing an adequate job of protecting you against infectious agents.
Skin biopsies from fibromyalgia patients show mast cells are activated and spewing out chemical irritants.4 Whether this leads to a higher frequency of skin infections in fibromyalgia is unclear, but these protective cells are disrupted. Indeed, the skin appears to be an immunological battleground with elevated levels of IL-1, IL-6, and TNF.5 These substances cause pain and may be why the skin’s concentration of opioid receptors (delta and kappa, but not mu) is through the roof.6
GI Barriers Impaired
Mast cells are just one of many cell types that line your gastrointestinal (GI) tract. A healthy GI lining prevents bacterial products from entering your system. However, the composition of gut bacteria is unfavorably altered in fibromyalgia.
Species that strengthen your gut lining are depleted and your intestinal permeability is enhanced.7 But that’s not all. Microbial products from the gut are elevated in the blood of patients with fibromyalgia, promoting an inflammatory state and possibly impairing your body’s ability to kick infections to the curb.
Immunoglobulins
Antibody-containing immunoglobulins are in the low to low-normal range in fibromyalgia patients, according to two separate studies. Immunoglobulins protect your body against infectious agents and low levels make you more vulnerable to all sorts of pathogens.
In one study, seven different types of immunoglobulins were measured, and 96 percent of fibromyalgia patients were low in at least three of them.8 In addition, higher rates of sinus infections corresponded with reduced immunoglobulin levels. A second study confirmed that the two most common immunoglobulins are decreased in fibromyalgia patients compared to healthy subjects.9 In other words, this finding is not a fluke.

Complement System
Your complement system is composed of important proteins involved in your body’s defense against infection. This system is also activated in autoimmune and chronic inflammatory diseases such as rheumatoid arthritis. A recent report shows the complement system is excessively activated or on high alert in fibromyalgia patients.9
While the complement system helps eliminate pathogens, chronic activation leads to immune system imbalances. This leaves fibromyalgia patients more vulnerable to infections. Also, an overly active complement system reduces the integrity of the blood-brain barrier. And when this happens, immune cells in your brain are triggered into action, causing neuroinflammation.
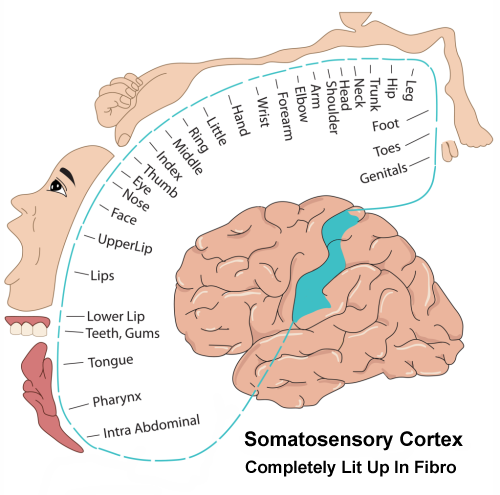
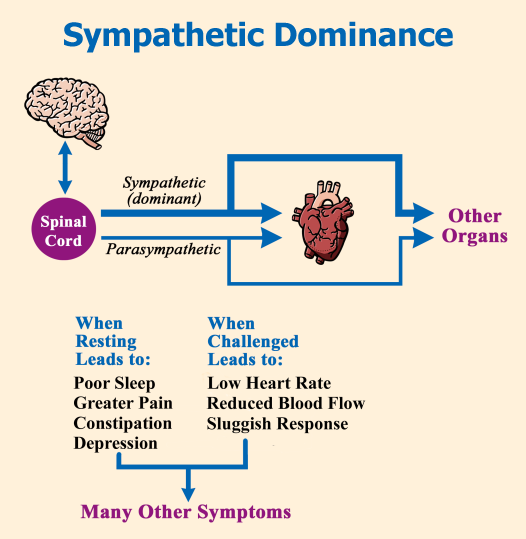
Altered Brain Response
With so many immune disruptions throughout your body, it’s impossible for the immune cells in your brain to be “chill.” Several imaging studies, including one funded by AFSA, document neuroinflammation in fibromyalgia patients. In other words, the microglia cells in your brain are on high alert and pouring out chemical distress signals.
It’s well documented that your brain does a poor job of controlling pain, regulating sleep and performing cognitive tasks. And when it comes to responding to infections, an AFSA-funded study shows the brain heats up, pumps out more reactive chemicals, and reduces blood glucose levels. Rather than helping, this altered response impairs the brain’s ability to control infections in fibromyalgia.
Preventive Measures
Just knowing you are more prone to infections can help you prevent their detrimental impact. However, if you succumb to a pathogen, seek prompt medical care and get extra rest.
Aside from powering up your immune system with a good night’s sleep (as best as you can with fibromyalgia), consider the following proactive measures:
Reduce Stress – It drains energy you don’t have and depletes your immune system.
Regular Gentle Exercise – This improves the circulation of immune cells and it relieves stress. However, avoid straining your upper respiratory system. See Fibro-Friendly Exercises.
Hot Water Therapy – Tight chest wall muscles in fibromyalgia impedes lung expansion and this promotes more upper respiratory infections.10 However, regularly submersing the body up to the shoulders in hot water improves fibromyalgia pain as well as lung function.11 In addition, it reduces proteins in the blood that cause inflammation.
Irrigate Nasal Passages – Routinely use saline-containing nasal sprays to flush irritants, mucus and bacteria from your nose.
Protect Your Ears – If you are prone to outer ear infections from getting your ears wet, use Silly Putty (in the pool, shower or at the hair salon). If you get frequent inner ear infections, acid reflux during the night might be a contributing factor. Eat dinner at least two hours before bedtime and take an antacid before sleep (if it doesn’t interfere with your medications).
Floss Regularly – This decreases your risk of gum infections.
Eat an Anti-inflammatory Diet – Reducing foods that disrupt your intestinal lining can ease digestive symptoms and reduce systemic inflammation.
Low-Dose Naltrexone (LDN) – LDN works on a variety of immune cells to decrease the production of inflammatory cytokines and reduce neuroinflammation in the brain. Unfortunately, it takes one to three months to show symptom improvements. See our article: Giving LDN Your Best Shot.
Research & Fibromyalgia Infections Resources
Stay Current on Treatments & Research News: Sign up for a Free Membership today!
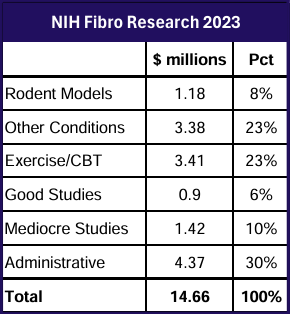
Research holds the key to better treatments. AFSA funded three projects in 2024; help us fund more in 2025.
Diagnosis | Symptoms | What Is Fibro | Finding A Doctor | Muscle Pain Relief
- Vinker-Shuster M, et al. Biomedicines 12:2821, 2024. Free Report
- Sheng-Kai Ma et al. J Periodontal 93(6):877-887, 2022. Free Abstract
- Verma V, et al. PAIN 163(7):e821-e836, 2022. Free Report
- Blanco I, et al. Clin Theumatol 29(12):1403-12, 2010. Free Abstract
- Salemi S, et al. J Rheumatol 30(1):146-50, 2003. Free Abstract
- Salemi S, et al. Arthritis Rheum 56(7):2464-66, 2007. Free Abstract
- Martin F, et al. Front Immunol 14:1253121, 2023. Free Report
- Caro XJ, Winter EF. Clin Exp Rheumatol 40(6):1076-83, 2022. Free Report
- Izuno S, et al. BioPsychoSocial Med 19(1):1, 2025. Free Report
- Ortiz-Rubio A, et al. Expert Rev Respir Med 15(9):1217-27, 2021. Free Abstract
- Chadwick AL, et al. Front Pain Res 6:1526491, 2025. Free Report